Red meat allergy caused by ticks may cause digestive symptoms only : Shots
[ad_1]

A Lone Star tick (middle) flanked by a deer tick (left) and a dog tick. The Lone Star tick is thought to be primarily responsible for an allergy to red meat, but other ticks can’t be ruled out.
Getty Images
hide caption
toggle caption
Getty Images

A Lone Star tick (middle) flanked by a deer tick (left) and a dog tick. The Lone Star tick is thought to be primarily responsible for an allergy to red meat, but other ticks can’t be ruled out.
Getty Images
There’s an increase in emergency department visits for tick bites this time of year as people spend more time outdoors. Increasingly, these bites are linked to illness, everything from Lyme disease to babesiosis. And, there’s another emerging risk linked to tick bites known as alpha-gal syndrome, which causes a red meat allergy.
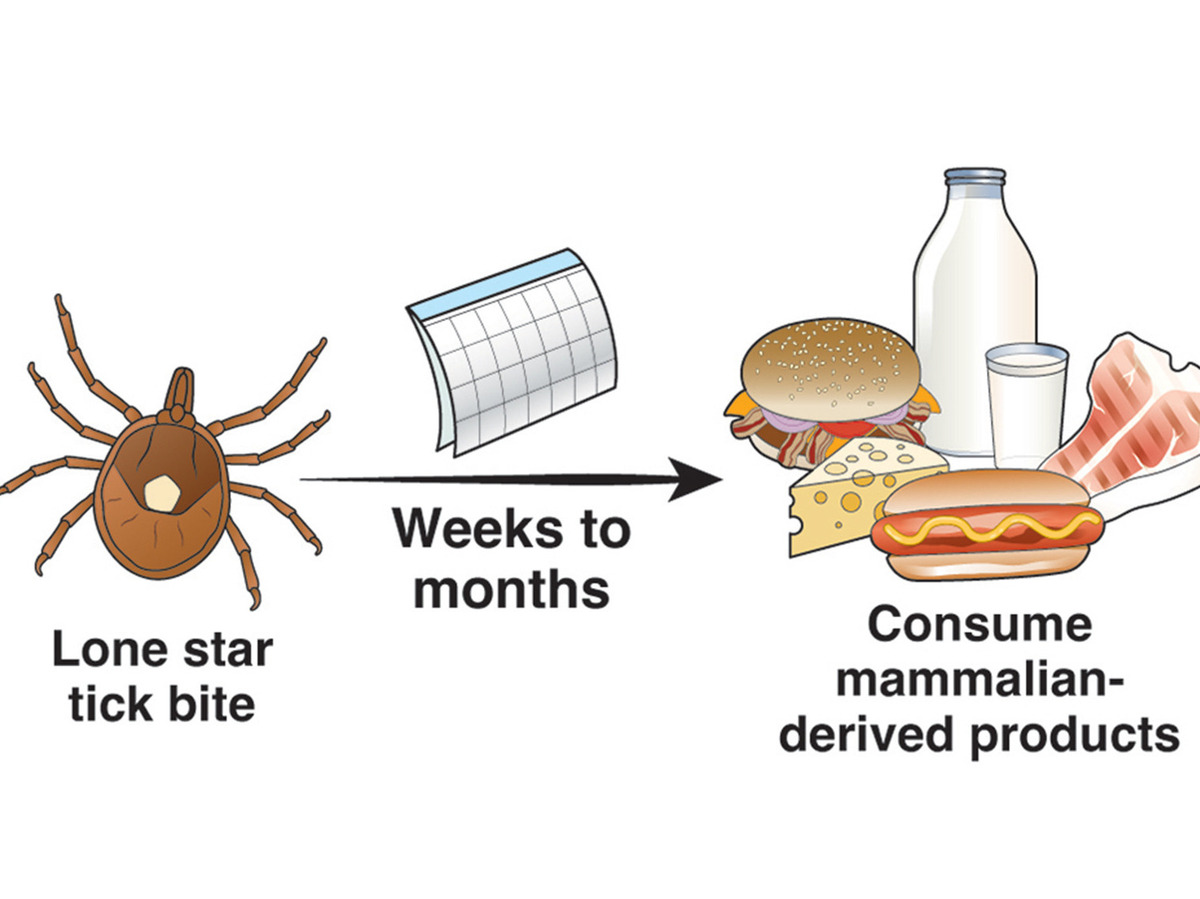
Scientists first connected the dots between red meat allergies and tick bites more than a decade ago, when they identified patients who got allergic reactions such as hives or anaphylaxis after eating beef or pork. Most had been bitten by Lone Star ticks.
Now, doctors’ understanding of these allergies has evolved.
“What’s new is that we have patients who really just have GI symptoms,” explains Dr. Sarah McGill, a gastroenterologist at the University of North Carolina. McGill says some alpha-gal syndrome, or AGS, patients feel sick to their stomachs after they eat red meat, but never develop more typical allergic symptoms, such as a rash, swelling or trouble breathing.
McGill has co-authored new guidance for the American Gastroenterological Association to raise awareness about the GI-only onset. She has diagnosed AGS in people who experience abdominal pain, diarrhea, nausea or vomiting about 2 to 6 hours after eating red meat.
That’s exactly what happened to Randy Rayborn, 72, who lives in a rural community in Caswell County, North Carolina. “I figured it was food-poisoning,” Rayborn recalls thinking after his first alpha-gal attack in the fall of 2019. “I woke up in the middle of the night with severe pain and nausea. I had to rush to the restroom,” Rayborn recalls.
He describes the episode as “the most violent upheaval” he’d ever experienced.
Deer and ticks are prevalent near Rayborn’s home. He recalls pulling several ticks off his body in the months before his illness began, but he didn’t realize the bites had triggered the illness. Nor did he imagine that the hamburgers or bacon he’d eaten had anything to do with it.
When he had a similar attack a few weeks later, he went to see his doctor, who referred him to McGill. A blood test showed he had Immunoglobin E, or IgE antibodies to alpha-gal, the sugar molecule that he was exposed to from the tick bites, suggesting he was positive for the allergy. “I’d never heard of it,” Rayborn says, so he was very surprised.
McGill advised him to eliminate all red meat from his diet. “I miss bacon, I miss hamburgers, ” Rayborn says. But after suffering through such painful episodes, “I don’t miss them that much,” he says. He remains symptom-free after several years on the diet.
Alpha-gal is a sugar molecule found in most mammals, including cows, lambs and pigs. It can also be found in the saliva of ticks. Humans don’t make alpha-gal, so it’s foreign to us, explains Dr. Scott Commins, an allergist at the University of North Carolina in Chapel Hill. When tick saliva goes through a person’s skin and transmits alpha-gal it can be a potent inflammation trigger.
“Our immune system can be tricked into making an allergic response to this sugar,” says Commins. Then, after a person is sensitized to alpha-gal, they can get a reaction every time they eat red meat. Alpha-gal can be found in beef, pork, lamb, rabbit, deer meat as well as other products from mammals including milk and gelatin, according to the CDC.
Commins has published a new research paper on tick bites and the risk of developing the alpha-gal allergy. People who get multiple tick bites (four or more) and spend a lot of time outdoors in wooded areas are at higher risk.
And the new recognition that AGS leads some people to have only GI symptoms, without any traditional allergic symptoms, is a paradigm shift. “It was a surprise,” he says. Blood tests show that these patients have the same allergic antibodies as other AGS patients. “We did not know that we were missing these patients,” Commins says.
During her medical training as a gastroenterologist, McGill says she was taught that allergies don’t present with GI symptoms alone. But her clinical experience treating patients who didn’t experience any hives or rashes led her to a different conclusion. “This flies in the face of what I learned about GI distress and allergies,” McGill says.
Her change in thinking came after she saw a patient, similar to Randy Rayborn, who had experienced several episodes of nausea and GI distress. Each time it happened a few hours after eating a hamburger. “I did an endoscopy on that patient and it was normal,” McGill says. But a blood test showed the patient was positive for AGS.
“I started checking for it more often,” McGill says and she identified a string of patients who were also positive for alpha-gal antibodies. She advised all of them to go on the Alpha-Gal Elimination Diet.

American Gastroenterological Association
American Gastroenterological Association
Early in the pandemic, when her endoscopy lab was shut down, she had time to do some research and check in with patients she’d diagnosed with AGS. She found that patients who had eliminated red meat told her they felt better. They also reported getting sick again if they went off the elimination diet. “I was surprised,” she says. It was a confirmation that her diagnosis had been correct, and that avoiding these foods was an effective treatment.
Cases of alpha-gal syndrome have been concentrated in southeastern states, but the range extends from New York and Iowa to Texas and Florida. There have been cases reported on every continent (except Antarctica), and doctors say other types of ticks, beyond the Lone Star tick, may cause the syndrome.
A report in the New England Journal of Medicine, documents the case of a 47-year-old man in Ann Arbor, Michigan who stumped doctors in the E.R. who were not familiar with the condition.
In the new guidelines for gastroenterologists, McGill and her colleagues say it’s important for GI doctors to be aware of alpha-gal Syndrome and “be capable of diagnosing and treating it in a timely manner,” pointing to the importance of the elimination diet. The evidence from recent studies show roughly 75% of AGS patients improve when they follow an alpha-gal–avoidance diet.
[ad_2]
Source link