Interleukin-18 Signaling Pathway Promotes Activation of Hepatic Stellate Cells in Mouse Liver Fibrosis
The cytokine interleukin 18 (IL-18) was originally described as an interferon gamma (IFNγ) – inducible pro-inflammatory factor in septic shock models, which stimulates T-cell proliferation. Like IL-1β, IL-18 belongs to the IL-1 superfamily and is synthesized as a biologically active 24-kDa precursor protein (pro-IL-18) that lacks the signal peptide required for secretion. An intracellular cysteine protease called caspase-1, also known as il-1 beta convertase, cleaves pro-IL-18 into a mature active form.
NLR family pyrin domain containing 3 (NLRP3) inflammasome activation has been shown to lead to liver fibrosis. Mechanisms and downstream signaling remain incompletely understood.
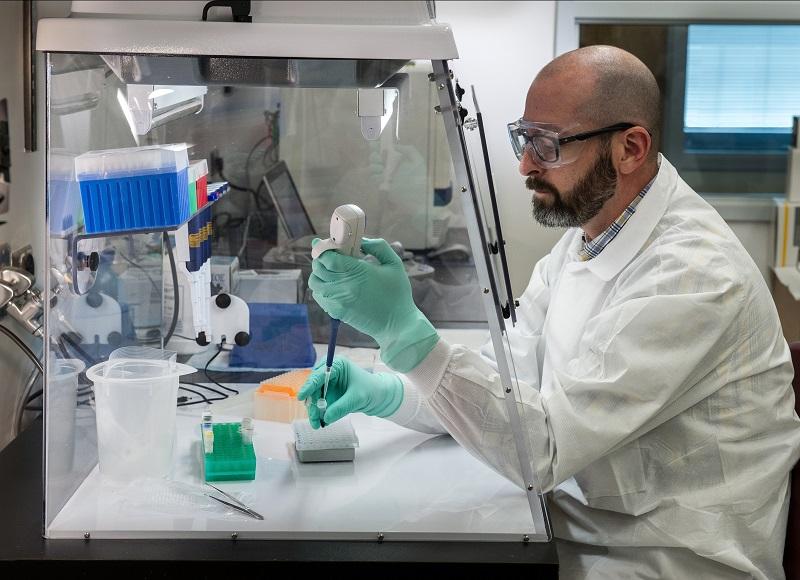
In this study, the researchers investigated the role of interleukin 18 (IL-18) in hepatic stellate cells (HSCs) and its effect on liver fibrosis.
Recently, scientists from Germany published an article entitled “Interleukin-18 signaling promotes activation of hepatic stellate cells in murine liver fibrosis” in Hepatology, which emphasized the role of IL-18 in the development of liver fibrosis and identified IL-18 as a new target for the treatment of liver fibrosis through its direct effect on HSC activation.
In this study, the investigators observed IL-18 (128.4 pg/ml vs. 74.9 pg/ml) and IL-18 binding protein (BP; 46.50 ng/ml vs. 15.35 ng/ml) in serum. Single-cell RNA sequencing data showed that immunoregulatory subsets of mouse hematopoietic stem cells expressed IL-18 and IL- 18 receptors. Treatment of cultured primary mouse stellate cells with rmIL-18 accelerated their transdifferentiation into myofibroblasts.
In vivo, IL-18 receptor-deficient mice reduced hepatic fibrosis in a model of hepatic fibrosis induced by hsc-specific NLRP3 overactivation. Whole liver RNA sequencing analysis of a mouse model of severe nash-induced fibrosis by feeding a choline-deficient, l-amino aciddefined high-fat diet showed significant upregulation of genes associated with Il18 and its downstream signaling, and Il18-/- mice receiving this diet for 10 weeks showed protection from fibrotic changes, with a decrease in the number of α sma-positive cells and decreased collagen deposition.
HSC activation triggered by NLRP3 inflammasome activation was abrogated when IL-18 signaling was blocked by its naturally occurring antagonist IL18BP. The investigators observed a severe inflammatory phenotype associated with myeloid cell-specific gain of Nlrp3 function that was rescued by IL-18BP.
In conclusion, the results presented here highlight the critical role of IL-18 signaling in the development of liver fibrosis through activation of hematopoietic stem cells in vitro and in vivo in three different mouse models. Blocking IL-18BP, as well as potentially other methods such as neutralizing antibodies, may provide a novel therapeutic strategy for the treatment of liver fibrosis.